Ectopic Pregnancy: Symptoms, Risks, Causes
Ectopic Pregnancy
Obie Editorial Team
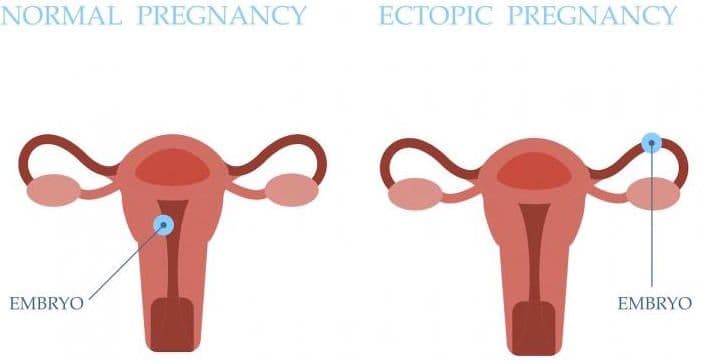
An ectopic pregnancy occurs when a fertilized egg implants and starts to grow outside of the uterine lining. These pregnancies most commonly occur in the fallopian tubes, but other implant locations do happen:
- In the fallopian tube (tubal ectopic: isthmic/ampullary/fimbrial)
- In the cervix (cervical ectopic)
- In the ovary (ovarian ectopic)
- The abdomen (abdominal ectopic)
- The corner of the uterus (cornual ectopic)
- Previous cesarean scar (scar ectopic)
It's crucial to recognize that ectopic pregnancies pose significant health risks, including severe bleeding which can be life-threatening if not immediately treated. The potential to carry an ectopic pregnancy to term is exceedingly rare, although in some rare cases, an undetected abdominal ectopic pregnancy can lead to a live birth.
Recognizing the Symptoms of an Ectopic Pregnancy
The symptoms usually become evident between 5 to 7 weeks after conception and can include:
- Missed period
- Positive pregnancy test
- Spotting
- Lower abdominal and pelvic pain, which may be predominantly on one side
- Vaginal spotting or mild bleeding
- Painful urination
- Pain during bowel movements
As the condition progresses without intervention, more severe symptoms like intense abdominal pain and heavy bleeding may emerge, indicating an urgent need for medical attention.
Exploring the Causes of Ectopic Pregnancies
About 1-2% of pregnancies are ectopic, primarily due to fallopian tube damage or blockages, impairing the fertilized egg's journey to the uterus. Other contributing factors include maternal age, history of pelvic inflammatory disease, previous fallopian tube surgeries, or fertility treatments.
Identifying Risk Factors for Ectopic Pregnancy
Key risk factors include:
- History of prior ectopic pregnancy
- Presence of an IUD
- Past pelvic inflammatory disease (PID)
- Aged over 35 years
- Smoking habits
- Endometriosis
- Previous tubal ligation
Contrary to some beliefs, prior induced abortions are not linked to increased risks of ectopic pregnancies.
Testing and Diagnosis
A vaginal ultrasound coupled with hCG testing is typically used to diagnose an ectopic pregnancy. In a normal uterine pregnancy, hCG levels double approximately every 48 to 72 hours, whereas in an ectopic pregnancy, this pattern is disrupted. Laparoscopy may also be employed, though it’s less common due to associated costs and risks.
Early intervention before rupture is critical, but even with vigilance, immediate care is essential if a rupture occurs.
Seeking Medical Care for Ectopic Pregnancies
If you've had an ectopic pregnancy in the past, informing your healthcare provider early in subsequent pregnancies is vital due to an increased recurrence risk. Report any unusual symptoms promptly for assessment and intervention.
Recognizing a Ruptured Ectopic Pregnancy
If a fallopian tube ruptures, you may experience sharp, stabbing abdominal pain and significant internal bleeding. This situation requires immediate medical attention.
Treatment Options for Ectopic Pregnancy
Depending on the stage and location of the ectopic pregnancy, treatment can include:
- Medication (Methotrexate)
- Laparoscopic surgery to remove the ectopic tissue
- In some cases, abdominal surgery or laparotomy
Future Pregnancies After an Ectopic
Experiencing an ectopic pregnancy can increase the likelihood of complications in future pregnancies, including a higher risk of recurrence, preterm birth, low birth weight, and placental issues. However, with proper management and monitoring, many individuals go on to have successful pregnancies.